5% of all patients we see will have a Binocular Vision Anomaly. It is important we are properly screening for it and not skimming over it.
First step
- Observe the patient, head tilt? Walking funny?
- Rule out pathology – check the pupils, ophthalmoscopy and visual field defects
- General history and symptoms, medications?
- Family history of strabismus, amblyopia, refractive error or pathology?
- Recent headaches or trauma?
- BV anomalies can be comitant or incomitant and heterphoric or strabismic.
NOTE:
Incomitancy = when the angle of deviation is not the same in all positions of gaze
Comitancy = when the angle of deviation is the same regardless of position of gaze
Heterophoria = when the eyes are dissociated there is lack of fusion. It is also known as latent strabismus
Strabismus = Abnormal alignment of the eyes
If a patient is comitant and has a strabismus do they have a sensory or motor fusion issue? Are they amblyopic? Check
their visual acuity (VA). Three per cent of children are amblyopic. If they are amblyopic is it strabismic or anisometropic?
How to examine Binocular Vision Anomalies
- Cover/Uncover
- Ask the patient to look at a letter 1 line above the patient’s worst
eye’s best VA. - Look at the uncovered eye when covering the other eye.
- If when covering one eye, the other eye moves in – it means it WAS OUT and therefore the patient has an EXOTROPIA and vice versa for an esotropia
- If neither eye moves, check for heterophoria
- This time, look at the covered eye when you remove the cover. If it moves out it WAS IN, hence the patient has an ESOPHORIA and vice versa for an exophoria
- NOTE: Don’t do test too slowly, record the size of the deviation, do aided and unaided
- Ask the patient to look at a letter 1 line above the patient’s worst
- Alternating Cover Test
- Allow angle of deviation to build up (and to completely dissociate takes around 6 cover/uncover repetitions)
- Be aware that an alternating cover test makes phorias and tropias look the same. You need to do a basic cover test to determine between phoria and tropia and this test is used to check for phorias after ruling out a tropia.
- NOTE: Estimating the size of deviation– Get the patient to look at the 6/12 line, ask them to focus on the first letter and then look quickly at the last letter. The distance from the first to last letter is around 12 cm and the eye movement from the beginning to the end is around 2 prism dioptres.
- Motility (checks if the deviation is
incomitant)- With a pen torch shine the light so both corneal reflexes can be seen (around 35cm from the patient).
- Are the corneal reflexes aligned? If they are not aligned the patient will experience diplopia.
- Ask the patient to follow the light with their eyes but to keep their head still
- Move the pen torch in either H or star pattern (whichever you
prefer) - Repeat the test and this time ask if they experience any double vision or pain
- If they experience double vision, is it horizantal or vertical?
- If horizontal, a horizontal muscle is underacting and if
vertical, a cyclovertical muscle(s) is/are underacting - NOTE: If after cover test and motility you suspect incomitancy,
do a hess chart - Incomitancy = when the angle of deviation is not the same in all positions of gaze
- Comitancy = when the angle of deviation is the same regardless of position of gaze
- Convergence
- After the near cover test use a detailed target to ensure accurate accommodation.
- Ask the patient to bring the target inwards as close to them as possible and then measure the distance when the target is blurred or two
- This tests for any convergence insufficiency
- This test is relevant for patients with phoria
- Poor convergence can be associated with de-compensated near EXOPHORIA
NOTE: detailed targets for accommodation measured in cm. Normal <8cm Abnormal >15cm. Accommodation and convergence issues can co-exist. Poor accommodation is a sign of latent hypermetropia which would then be a reason to conduct a cycloplegic refraction.
- Amplitude of Accommodation
- Test one eye at a time.
- Ask the patient to bring random words close until they become blurry. Measure the distance.
- Bring words back until they become clear again. Measure the distance.
- The average of these two distances = Amplitude of accommodation
- Mallet Fixation Disparity This test is great for assessing heterophoria
- Some patients are asymptomatic and have fixation disparity BUT it may make stereo acuity worse/reduced and make the visual system under stress
- Fixation Disparity can also mean that a heterophoria is decompensated
- Instructions
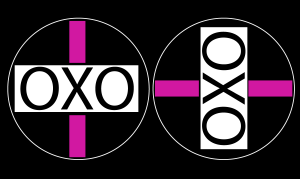
- OXO=Central fusion lock I = peripheral lock
- Increase room lighting
- Patient is to put on polarised glasses
- Hold mallet unit at their normal reading distance (Left OXO diagram used to check for horizontal heterophoria and Right OXO diagram used for vertical heterophoria)
- E.g for checking horizontal heterophoria:
- Check that they can see OXO with pink line above and below. Concentrate on the X, ask them if the lines have moved?
- If top line has moved to the left, the RE has deviated outwards (R XOP)
- Introduce BASE IN prism in stages.
- When prism is introduced ask the patient to read text to refocus
- An aligning prism of less than 1 prism dioptre is ok.
NOTE: In pre presbypoes 1 prism dioptre is normal. In post presbyopes 2 prism dioptres is normal. If above, the patient will likely have symptoms of a decompensated heterophoria.
- Foveal suppression
- If a patient has a decompensated heterophoria the binocular system comes under stress. Due to this, an area at the fovea may become suppressed (not seeing)
- The near Mallet Unit is used to measure foveal suppression
- The patient is wearing polarised
lenses - This test assesses what each eye is able to see
- HAND HELD NEAR MALLET UNIT TEST
LE should see Both eyes should see RE should see TH THO HO LO LOA OA AH AHT HT HAOE HAOETL OETL - The eye which reads the furthest down should be covered (with the polarised lens still in place)and then the other eye checked again.
- If the patient can now read 2 lines lower on the unit = significant foveal suppression
- If the patient reads only 1 line or less lower = normal
- Stereopsis (Stereoacuity) tests include:
- True Random Dot test
- Very good at detecting strabismus
- If patients don’t see targets, they are very likely to have a squint
- Contour tests e.g Titmus/Fly test
- The patient has to identify which shape is lifted up from the page
- This is not so good for strabismus, however if they manage to see the very small pictures they are unlikely to have a squint or heterophoria
- True Random Dot test
- Fusional Reserves (FR)
- FR is the measure of how much convergence and how much divergence a patient has in reserve
- Test normally done at near
- Ask the patient to look at an accommodative target (e.g a letter)
- Measure FR that oppose heterophoria first for e.g XOP use base OUT prism (this forces the patient to converge as much as possible – Positive FR)
- Increase prism in 1 dioptre intervals
- Ask the patient to tell you when the letter becomes blurred or doubled
- Record results as
- BLUR POINT e.g 12
- BREAK POINT e.g 18 D (when doubles and convergence
fails) - RECOVERY e.g 14 D (when px gets back to single
when prism is reduced again)
- Then turn the prism around and do base IN – this time making the eyes diverge (negative FR) NOTE: Negative FR are generally much weaker than positive FR
The next article will be focusing more on diagnosing BV anomalies and especially how cranial nerve palsies can affect BV




