Age related macular degeneration (ARMD) is the definition for damage caused at the macular. The macular is located in the central area of the retina and is responsible for detailed vision. Therefore, damage to this area can cause profound vision loss and significantly affect a person’s quality of life. Age is the main risk factor and normally patients present with this condition when they are aged 60 or over. Around 1 in 10 people aged 65 and over show some signs of ARMD.
ARMD can be categorized into 2 types. DRY ARMD (non – neovascular) and WET ARMD (neovascular)
Dry ARMD
Dry ARMD is the most common type and as previously mentioned, is very related to age. Other risk factors include family history of the condition, being female, having blue eyes, smoking and being exposed to a lot of UV light.
How does it happen?
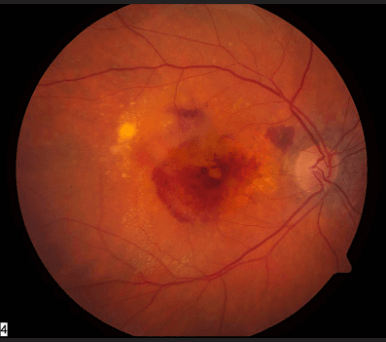
Why ARMD occurs is poorly understood but what we do know is as we age, extracellular breakdown deposits called “drusen” occur within Bruch’s membrane. Bruch’s membrane is the thin layer that separates the retinal pigment epithelium (RPE)/Retina from the underlying choroidal blood supply. The drusen clogs up the area, making it difficult for the choroid to supply the retina with nutrients. In addition to this, the waste products from the photoreceptors are unable to drain freely down into the choroidal bed. This degeneration of retinal pigment epithelium (RPE) cells and photoreceptors occur in the later stages of dry AMD and is also known as geographic atrophy (GA). Examination may show drusen or areas of hyper-hypo RPE and can correlate with varying degrees of vision loss. Dry ARMD takes many years to progress but it is a chronic disease where most patients have some level of vision impairment. Sometimes it can progress to severe blindness and this is where low vision assessments become very important.
Wet ARMD
Wet ARMD is less common but can be much more severe. It is important to detect it early as unlike Dry ARMD, it can be treated. Wet ARMD can result from progression of Dry ARMD but it can also occur spontaneously.
How does it happen?
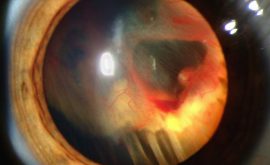
Wet ARMD is typified by choroidal neovascularization (CNV). A break in Bruchs membrane causes new weak blood vessels to grow towards the outer retina from the underlying choroid. Due to the weakness of these vessels, they can leak fluid below or within the retina. This is serious because the leakage occurs at such a sensitive area for sight. If left untreated, these leaky areas can scar over, causing catastrophic vision loss .
Treatment
Dry ARMD
Dry ARMD can not be treated but there are things that can be done to help slow done progression. This includes UV protection, ceasing smoking, eating leafy green vegetables and taking certain vitamin supplements. Patients must also be encouraged to self monitor their condition using an AMSLER CHART. This is a small grid which is used to check for any distortion or metamorphopsia (presence of wiggly lines). The patient is instructed to cover one eye and then the other, whilst wearing their near vision correction. Assessing each eye individually, if lines appear wiggly/wavy or there are significant areas of the grid distorted or missing the patient should visit their Optometrist or hospital eye service immediately to get checked for progression of Dry ARMD into Wet ARMD. Metamorphopsia in particular is a red flag for Wet ARMD as this can indicate fluid development at the macular (macular oedema).
Wet ARMD
Wet ARMD is treated using:
- Lucentis Injections
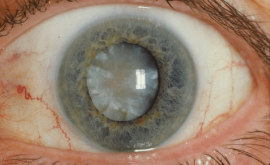
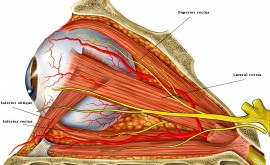
This is commonly done and has proven to be a successful method of treatment. Lucentis or Avastin are anti-VEGF drugs that are injected into the vitreous humour of the eye to stop the growth of new, weak blood vessels (neovascularisation). It also helps decrease vessel leakage, reducing macular oedema.
- Photodynamic Therapy (PDT)
This involves injecting a special chemical into the blood which reacts to wavelengths of light. Once the chemical is floating within the retinal blood vessels, light of a specific wavelength is focused directly at the vessels in order to coagulate the weak blood vessels. The idea here is that the leakage is stopped without affecting the surrounding retina. However, this technique is has proven not to be the most successful and is done less nowadays.