A cataract is simply defined as a haze or clouding of the natural crystalline lens of the eye. They are very common and in the western world, are the most common cause of vision loss in the over 40s.
The natural crystalline lens mainly consists of water and protein. It is made up of three important parts 1. The inner nucleus 2. An outer cortex 3. An outer shell known as the lens capsule. As we age, the outer cortex of the lens continues to grow. Some have described it to be like an onion, increasing layer by layer over the years. This increase in size changes the consistency of the lens where there is a build up of insoluble protein. Depending on where it accumulates, determines the type of cataract.
However, cataracts can form as a result of disruption to the lens. For example some children are born with them (known as congenital cataracts) or trauma, excessive UV light, toxins (e.g too much alcohol, smoking or sometimes overuse of steroids) may cause them prematurely. Also, having a metabolic condition such as high blood pressure, high cholesterol, diabetes or another eye condition such as high myopia can speed up the onset of a cataract.
The most common types are summarised below:
Nuclear Cataract – most common type and this is where the very central, inner nucleus of the lens becomes hazy. This is called the age related type.
Posterior Subcapsular Cataract – this is also common and related to age. However, this type of cataract can be associated with steroid use. The haziness occurs at the back of the lens.
Cortical cataract – these occur in the cortex of the lens due to changes in the water content of the lens fibres. As a result, the cataract appears as little spokes around the cortex, like the spokes of a bicycle wheel.
NOTE: Cataracts can be mixed where more than one type occurs. This is called ‘combined cataract’.
Signs and symptoms of cataract
Early cataracts often have no symptoms at all. However, normally patients initially present with difficulty driving at night or the glare from oncoming headlights. Depending on the type of cataract, the symptoms can vary. For example:
Nuclear Cataract: some patients experience an improvement when reading and this can sometimes be due to a ´myopic shift´ in their refraction which in turn, may indicate a nuclear cataract.
Posterior Subcapsular Cataract: Patients notice their vision is troublesome when reading due to the haze presenting at the back of the lens known as the ‘nodal point’ of the eyes lens system. Even if these cataracts don’t appear significant, they can be very symptomatic.
Treatment of cataracts
The treatment of cataracts depend on the severity of the cataract. If they are mild, a change in spectacle prescription may be sufficient. Also, additional lighting may help whilst reading. However, if the vision can no longer be improved with spectacles or perhaps the patient is very symptomatic, surgery is the best option.
This surgical procedure has become more and more sophisticated over the years. It is quick and usually very successful where most patient’s vision (around 90%) is restored to a great level. However, as with any operation, complications may occur. These include:
- Inflammation (normally mild an subsides)
- Infection (rare)
- An increase in floaters (although these often subside)
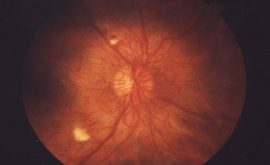
- Retinal detachment (rare)
- Tearing of lens capsule during surgery (rare)
- Posterious subcapsular opacification ( quite common but not serious – this is due to a thickening of any residual lens membrane. It can happen months or years after surgery but is easily resolved by a painless procedure called YAG laser)
The ophthalmologist explains everything prior to surgery and then gives the patient an information leaflet with an outline regarding the procedure. Normally one eye is done, and if needed, the second eye is operated at a later date.
The procedure is as follows:
- Px is given a pre-operative appointment where Nurses take a series of measurements to aid the Ophthalmologist select the most appropriate Intraocular Lens (IOL).
- The patient then returns around a week later for surgery.
- Initially, the eye is cleaned and anesthetised using eye drops.
- The Ophthalmologist then lies the patient flat, clamps the eye and makes a small 2-3.5mm incision (this is all completely painless)
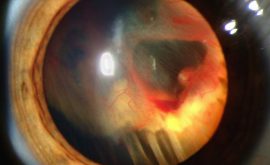
- A small probe called a phacoemulsifier is inserted through the incision which emits ultrasound waves.
- These waves break up the cataract but leave the lens capsule untouched.
- The same probe acts as a hoover and sucks up the broken up cataract, leaving an empty capsule.
- Into this capsule, the new IOL is folded and inserted through the tiny incision.
- The new IOL then unfolds and is positioned into the correct position inside the original lens capsule.
- At this point the surgery is completed and as only a very small area of cornea has been cut, no stitches are required.
- The px is then given some eye drops to keep the eyes lubricated and prevent any infection and inflammation
- The px can then leave after having a cup of tea and a little something to eat.
- The following day, the px returns and the surgeon checks for any signs of abnormality. If all is well, the px continues with the same drops for 2 weeks.
- After 6 weeks the Px then returns to see an Optometrist who re checks the eye for any signs of abnormalities and conducts a refraction in order to issue any required spectacles.
NOTE: Some px may not need any spectacles, it depends on the type of IOL inserted. However, many px may still need reading glasses, even if their distance vision is very good after surgery.